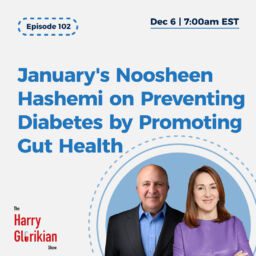
David Sable on the Genetic Revolution in Fertility Treatment
Episode Notes
David Sable got his start in reproductive medicine in the late 1980s, a time when he says fertility treatments were “very primitive.” But by the mid-2000s, he says, new procedures and new insights into the genetics of development had changed everything. His subsequent time observing (and investing in) the field has convinced him that reproductive medicine is “the most interesting area of medicine this century.”
Sable is a medical and entrepreneurial chameleon who trained in obstetrics and gynecology, worked as a reproductive endocrinologist, co-founded the Institute for Reproductive Medicine and Science fertility clinic, co-founded the embryo genetic testing firm Reprogenetics, and now works as portfolio manager of the Special Situations Life Sciences Fund and the Life Sciences Innovation Fund while also writing for Forbes and teaching biotech entrepreneurship at Columbia University.
Intriguingly, Sable says his earliest inspiration to become a medical entrepreneur came from the brief scene at the end of The Empire Strikes Back in which a robot clinician gives Luke Skywalker a prosthetic hand. To Sable, the seeming everydayness of the operation spoke to the possibility of “taking the miraculous and turning it into the mundane—taking the medicine and the science and along the way adding a lot of engineering to it.”
For more episodes on reproductive medicine and data please see episodes with Daniella Gilboa and also another with Alan Copperman
Please rate and review The Harry Glorikian Show on Apple Podcasts! Here’s how to do that from an iPhone, iPad, or iPod touch:
1. Open the Podcasts app on your iPhone, iPad, or Mac.
2. Navigate to The Harry Glorikian Show podcast. You can find it by searching for it or selecting it from your library. Just note that you’ll have to go to the series page which shows all the episodes, not just the page for a single episode.
3. Scroll down to find the subhead titled “Ratings & Reviews.”
4. Under one of the highlighted reviews, select “Write a Review.”
5. Next, select a star rating at the top — you have the option of choosing between one and five stars.
6. Using the text box at the top, write a title for your review. Then, in the lower text box, write your review. Your review can be up to 300 words long.
7. Once you’ve finished, select “Send” or “Save” in the top-right corner.
8. If you’ve never left a podcast review before, enter a nickname. Your nickname will be displayed next to any reviews you leave from here on out.
9. After selecting a nickname, tap OK. Your review may not be immediately visible.
That’s it! Thanks so much.
Transcript:
Harry Glorikian: Hello, I’m Harry Glorikian. And this is Moneyball Medicine. The show where we lead executives, entrepreneurs, physicians, and scientists using the power of data to reinvent healthcare from machine learning to genomics, to personalize medicine. We look at the biggest trends in patient care and healthcare management.
And we talked to people behind the trends to find out where data is making the biggest difference.
My next guest is someone who I would call a man with multiple identities. He’s a doctor, an entrepreneur, a professor and investor, and the list goes on and no, I’m not talking about Mr. Frank. Abignail from the famous movie. Catch me if you can. Although a movie of his life would be quite interesting.
Dr. David Sable, a long time friend of mine is indeed a genius, or at least for me, he is not only is he a certified gynecologist is also a successful entrepreneur, insightful university professor and writer for Forbes. Today. We are lucky to have him on the show and talk about his background and share his knowledge about entrepreneurship.
And most importantly, reproductive health. David is my go-to guy for reproductive health. Moreover, he shed some light on his perspectives and predictions regarding the current scientific landscape without further ado, Dr. David Sable.
Welcome to the show. Thank you for having me. David, you know, we’ve, we’ve known each other for a long time. Now, now that I’m thinking about it, it’s been a little bit of a while, and we’ve had the pleasure of sitting on a board together and so forth. And, but, you know, I, I want to start everybody off on the same level playing field of.
Of being always being fascinated by you and your background. I I’m always still in awe about these twists and turns that you’ve taken. Tell us a little bit about your background and how you started out your career and how you ended up where you ended up.
David Sable: Yeah, it’s a, it’s kind of, kind of a career brownie in motion.
Uh, if you started out, uh, earnestly studying accounting at the university of Pennsylvania as a fourth year of college, I decided to just take some sciences. I had taken no sciences. I finished all my degree requirements. So taking the path of most resistance that decided to take the entire pre-med curriculum while at the same time, just for the hell.
Harry Glorikian: Ah, no, no, no pressure. None whatsoever. Yeah, it was
David Sable: I was a senior it’s like I was in class with freshmen and sophomores and I found, I really liked it. Yeah, I, uh, applied to med school, not because I necessarily wanted to be a doctor, but I did want to be a medical student. I loved med school train that obstetrics and gynecology, which to me at the time was the best combination of medicine and surgery plus obstetrics, which it was a lot of fun.
Uh, around the time there were two Seminoles events that kind of really made the impression on me. One was a 1979 when the first IVF baby was born. Which to me seem absolutely revolutionary. And the other was a few months later, uh, interestingly, uh, towards the end of the movie, the empire strikes back.
You may remember Luke Skywalker got his hand cut off in a lightsaber dual with Darth Vader. And you’re wondering where this is going.
Harry Glorikian: Yeah. Yeah. I’m trying to think of, I can’t remember an IVF scene in that, but maybe I missed it.
David Sable: Well, there was no IVF, but it was, it was, to me it was the origin of thoughts or precision medicine.
Cause the next scene, after that Luke Skywalker sitting in a, in a table and I guess like a medical clinic in a robot is attaching his hat or a new hand. Right. And he attaches the hand and he pokes it a couple of times, Luke Skywalker looks at it, flexes the fingers, get up, gets up and kind of walks away.
What struck me about that was both incredible engineering. And I realized this was fiction,
Harry Glorikian: right.
David Sable: It was a phenomenal piece of engineering, but what was amazing to me was the nonchalance by which they just like did what would have been like just absolutely revolutionary medical procedure. And it occurred to me that you really, the future of medicine.
Was taking like the miraculous and turning it into the mundane.
Harry Glorikian Right.
Which was, yeah, you take the near the magic and you take the science and along the way you add a lot of engineering to it and it becomes kind of mundane and routine. So, uh, I trained in OB GYN in New York hospital where they had a phenomenal IVF unit and did a fellowship up at Brigham and Women’s in Boston.
And IVF was really in its early days. It was a lot of, you know, frankly, a lot of winging. It gave tremendous amounts of fertility, drugs, get as many eggs into the laboratory as you could fertilize, all of them make as many. Normal looking embryos as you can. And we weren’t all that good at it in the late eighties, early nineties.
So we would transfer three, four or five, six embryos to the uterus and hope that one stuck. Unfortunately when one stuck three or four of them often stuck. So you had triplets and quadruplets. And so it was real. It was kind of very early, very primitive medicine. And over the ensuing decade and a half in 1990 to 2004, I started an IVF program started two companies headed up a division. I really kind of watched as the science turned into a really great procedure. Yeah. The, uh, over, almost overnight, there were patient groups. We could do nothing for, you know, for example, what we call severe malefactor terrible, terrible, low sperm counts or no moving sperm.
And then, uh, the procedure, Dixie intracytoplasmic sperm injection was invented and overnight we were getting those couples pregnant as often as anybody else really terrific leaps and bounds. We went from just looking at the embryo and trying to divine what was going into it to being able to biopsy it.
And at first check for individual chromosomes, and then you carry a type the embryo, and now to sequencing.
Harry Glorikian: Right, right.
David Sable: Really just terrific, terrific stuff. Uh, Yeah. In 2004, I took a sabbatical, you know, we sold one of the companies that we would, we, uh, founded and we took our big hospital division at St.
Barnabas in New Jersey, private. And I thought it would be a good time to get to know my own children who barely knew their father was. So I took a one-year sabbatical for medical practice and a one year sabbatical was now in its 16th year.
Harry Glorikian: I feel like you pivoted back to that now I know, see the accounting thing I was missing now. I know how you know, all those numbers, so well,
David Sable: aha. Well, no. Okay. Accounting lasted one semester. It did love finance and economics and, uh, started studying healthcare, finance and economics, which helped a lot when we started starting companies. And while I was uh, doing my sabbatical. A friend who ran a large trading desk at Deutsche bank.
He asked me if I’d spend one afternoon a week there and he was running a quad strategy, which, you know, generate a large print out of go long. These stocks go short, these stocks. And he would say, you just go down the list and pick out whether you think the algorithm made mistakes. So, uh, I did that and these were 2004 level algorithms.
So it was relatively primitive and I guess I was adding enough incremental benefit that they kind of asked me to hang around full time. So I did. And before all of you, they gave me a little bit of money to invest myself and for Deutsche bank this was like the equivalent of the change behind the sofa cushions.
I wasn’t going to get anybody in trouble. Right. What I was investing and I think it was an opportunity to really learn how to invest. We did a deep dive into portfolio management was running at one point like six or seven different strategies and all preparing to go back in practicing medicine. Again, I’m going to cook a couple of heads. And one group offered me a job. And I said, thank you very much. I’m going to go back to practicing medicine. And they just kept coming back and making the offer more and more enticing. And finally, I figured out what the hell I’ll spend a year there. I’ll probably go back and medicine a year later and I’ve been there for 15 years now.
Yeah, so it’s so worked out. They haven’t thrown me out yet. And along the way I started teaching at Columbia started writing for Forbes. And just two years ago, I launched my first venture fund, which is a venture capital fund based. Yeah. Talk about full circle only on, in vitro fertilization, which was my old field.
Harry Glorikian: Total, total slacker, David total, total, total slacker, you know, and you tell me I keep busy, right? Which is funny because you’re way busier than I am.
David Sable: You somehow you have 40 hours each day, 38 of them. I’m stuck with the usual 24, but it’s a lot of fun. Very, a lot of interesting areas in reproductive medicine, I think is the most interesting area of medicine. This century.
Harry Glorikian: You know, it’s funny because honestly, like whenever anybody says anything, even coming within range of reproductive medicine, I’m like, hold on. I got to call David because you’re my go-to guy when it comes to this, because you can look at it sort of the way that I look at other stuff, which is totally under, you know, deep delving into the science, is this real?
Can it happen? But then at the same time, How do, is this going to make any money? Like, is this actually going to be a viable venture? Right. So it’s looking at those two through those lenses to make these decisions about what, to, what to think about going, you know, going into next. But I mean, and you were kind enough to introduce me to a couple of other guests, um, Daniella and, uh, Dr. Copperman, but you know, where do you see the biggest. Changes. I mean, the things that I got from, from him were I went into this it was surgery, and now, you know, it’s completely data driven. Uh, when I got from her was the torrent of data coming from all the different inputs is going through the roof. So it gives you more clarity about how to manage that patient.
Where do you see the biggest opportunities in the space from a, from a science perspective?
David Sable: Yeah, no, it’s a great question that a lot of thinking about it and, you know, taking a step back and just, you know, looking at healthcare in general, you know, we, we’re in a, I don’t know, 70, 75 year journey now from the pure analog to the digital within healthcare.
Even when I was in medical school, you know, in the late 1980s, you know, lung cancer was a tumor that was in the lung. Yeah. So, uh, and in, it was a couple that couldn’t get pregnant go to the year 20, 20 lung cancer is now subdivided and stratified to where we were characterizing these tumors down to the single amino acid mutation.
Almost and, and it’s, it’s, it’s agnostic to anatomic site. So we’ve truly become reproducible, very highly and precisely characterized, which lends itself to very predictable, uh, clinical study design. Which lends itself to predictable handicapable business plans and ecology now where lung cancer resides tens of billions of dollars of risk capital going into them. So it’s a truly, it’s truly a advanced part of precision medicine. Now, if you go back to the rest of medicine, there’s kind of a continuum between the pure analog clinical judgment and magic it. Know When I see it pattern recognition side, and then the really data-driven digital side. And on the data-driven side, you have oncology, you have inflammation, you have certain parts of surgery where robotics has made a huge difference.
And then you go back to the kind of more primitive side where yes, parts of, uh, psychiatry are, and neurology like brilliant people doing great work, but nature has not made it easy for us to study these dynamic processes and women’s health is a lot closer to the analog side than the digital side. When you look at the diagnoses that we have in women’s health things like preeclampsia, preterm, labor, dysmenorrhea, premenstrual syndrome.
Yeah, these are kind of pattern recognition that they’re very real, but we just don’t know where they’re coming from. You know, so we, we described them in these very vague terms and it’s very difficult to find treatments for them in fertility. Sadly, even though there are more things that we can look at more specific.
Functional States. Yeah. Function of sperm, egg maturation function, the fallopian tubes, uh, the uterine lining when it comes down to it, infertility is still pretty unexplained. So we are, you know, very much in a there’s a bit of a shotgun aspect to it, which is ironic because as you correctly pointed out, uh, there’s tremendous numbers of interventions in measurable stuff going on.
We take the egg and the sperm out of the body have fertilization happened in the laboratory and then have access to the dynamics of embryo development. So that’s going to kill area number one of interest in that area, area number two, which even surprised me when I went back and from a business standpoint, did a deep dive into reproductive medicine, and it’s probably the most undertreated under-penetrated area of medicine.
Particularly in the United States. And I got to throw some data at it and get some numbers because it seems counterintuitive because a lot of us know someone who’s been through IVF. There’s tremendous amounts of press covers a very popular thing to talk about. But if you look at the codes, compare it to oncology.
There’s 15 million people with cancer in the United States, and there’s about 7 million people within fertility. So about a two to one ratio, uh, Now people will say, well, one is cancer, which you could die from. But if you think about it, oncology, you suffer from between one and 12 years. It’s very life altering.
You go through areas of intense treatment and then periods of time, we do very little patients are extremely compliant, extremely motivated. Turn to look at the 7 million people with infertility. They typically suffer for between one and 12 years. It’s incredibly life altering, you know, having taken care of these patients for the decade and a half life is not bad, normal until they have a baby.
It really, yeah. It just completely puts everything else on hold. So you have tremendous motivation, tremendous compliance. And the size of the IVF economy in the United States is about arguably 4 to 5 billion. Yeah. That’s nothing. We have a two to one ratio of. People affected in a 20 to 1 ratio of the amount of money that goes into it.
But more importantly, if you’ve got cancer in the United States, at some point you get treated,
Harry Glorikian: Right?
David Sable: Yeah. Nobody’s going on, treated with cancer in fertility, we have 7 million people suffering from it, our best procedure IVF results in about 70,000 babies a year, which is about 1% of the people that suffer from the problem.
Or having the solution come up with an answer for them. That’s to me, that’s that number. I had to stare at that number an awful lot before I realized just how undertreated and under penetrated this fairly high profile high publicity procedure is no, I
Harry Glorikian: That goes to like, but I mean, there’s, there’s so many factors that may play into that. I mean, there’s. Insurance. There’s all sorts of things. Cause I wouldn’t, I was talking to Danielle, she was saying like in Israel, like we pretty much go until you’re pregnant, so more or less. Right. Um, and whereas here. That’s expensive. Yeah.
David Sable: And that’s what I, when I studied, uh, IVF usage internationally, uh, the data really bears that out. Israel, they do one cycle for about every 200 people in the country it’s paid for by the government until you’ve had two children, which is pretty remarkable. Uh, in the United States, we do one cycle approximately for every one and one cycle, probably 1700 people. An eight and a half fold difference Israel.
Harry Glorikian: Well, one is a national security issue.
David Sable: Well, it’s, regardless of what the regards to the inputs,
Harry Glorikian: Right,
David Sable: You’ve got a 8 to 9 fold difference in the U S we approximately 1.8% of the babies in the U S report from IVF. in Belgium and in Scandinavia, it’s closer to one and nine. So , Im sorry It’s closer to 9%.
We have about 2% versus 9%. Uh, we do twice the amount of IVF in Japan than we do in the United States per capita, three times the amount in, in, uh, in Spain. And it really comes down if you graph it against, out of pocket costs. It’s exactly, as you said, we just choose to live on a part of the demand curve.
That’s in the upper left side, fewer cycles at a very high out of pocket costs. And when I first looked at the industry, again, back in 2011, thinking, you know, I got to find a way to invest in this industry. That’s the first thing that struck and struck me, is that okay, there’s this great opportunity, but then you think, all right, well, what’s the catalyst that’s going to change that.
Yeah, we’re in a steady state, every IVF doctor, and I was one of them. They’re all making a good living. They’re all busy. There’s 486 IVF clinics in the United States. There’s 1300 specialists and they’re all doing a good job. The quality of care is very high, but there’s no innate motivation To go out and create a parallel industry at a lower price point, because right now the IVF industry is it’s like a hotel industry with nothing, but the Ritz Carlton in the four seasons, if you can afford a thousand dollars a night, you get an amazing night’s sleep.
If not, you’re buying, you’re sleeping on a friend’s couch.
Harry Glorikian: Yeah. I, and, and, but, but this is like, I mean, you and I both know this. Sometimes disruption has to come from outside because everybody’s comfortable in where they are.
David Sable: Exactly and that’s coming now since 2013, there’s been one after another cat catalyst in the U S that started to transform the industry.
Number one is that private equity discovered IVF, which is, yeah. kinda predictable. I, you know, private equity is industry agnostic. They look for high margins. Right. Decentralized low yet IVF. There’s no clinic. That’s got a majority of that owns a huge piece of the marketplace. So IVF private equity came in just about the time that people, my age, who started a lot of these big clinics were looking for exits.
So that was step one, step two. The US government started covering it for veterans. And started covering IVF and egg freezing for people with, uh, battle related injuries. That was very large. Uh, number three and probably most important is the human resource industry discovered that the single most important benefit for high cost of acquisition and high cost of retention employees was offering IVF coverage.
Previous to this, there was very little employer coverage for IVF. There were state mandates from state to state. I think there’s 14 of them. And these state mandates are very inconsistent from one state to the other. Some of them say, if you’re an employer and you provide coverage, it has to include IVF in others.
It was just kind of a, almost a face-saving gesture. But, uh, outside of the state governments, the companies themselves decided that it’s is a good business practices to start providing it. And you know, a lot of people may have seen a company called Progyny when public last year and in their public filings, they said they’ve got 1.4 million people under coverage for only for IVF and egg freezing coverage.
Now, if you apply a 10% prevalence of infertility on that 1.4 million people, that’s 140,000 people. Uh, many of whom had never, never had coverage before. And presumably couldn’t afford IVF. Yeah, up until recently, we’ve been treating 130, 140, 150,000 people a year with IVF. So we take a new, a new, a bolus of 140,000 newly insured people streaming into the marketplace. That’s pretty disruptive.
Harry Glorikian: We need to, maybe we need to open a new clinic. Uh, David, um,
David Sable: You need to open a new clinic, but it’s perfect. Lead into the point that I’m kind of, my thesis is not only going to open new clinics. We need to automate an engineer IVF. Right. We need to do IVF what we’ve done to some of these other automated process optimize and engineered areas of medicine so that we can scale it because IVF is kind of every IVF labs kind of like in our teasel kitchen, right?
You go in there, they’ve got their own way of doing things or honed, nomenclature, their own vocabularies. Some of them have standard operating procedures. Some of it just like it’s passed down, like, like legendary lower. From one embryologist to the next and in aggregate, it works pretty well, but that’s not a good way to scale an industry, right?
So this brings us to artificial intelligence, machine learning, and really we’ve had 40 years of great science and mediocre engineering. And it’s time to bring the engineering up to the level of the science. So that’s a very long winded answer your question.
Harry Glorikian: No, no, no, no, no, no. And, and, and it’s right. I mean, you know, I, I think to myself, I mean, all the areas are sort of spinning in my head of.
Well, we could do, you know, image analytics on that. And then you could, you know, all the temperature measurements that you get from women, you can start. I mean, there’s, there’s a ton of data to start working with. It’s just binning these in different categories to figure out which one is the ones to take forward.
And I know you’re constantly looking at companies in this area to see which ones have figured out a better mousetrap to drive forward on the data side. Um, and then of course, I’m, you know, I’m talking to people like Robert Green about doing, uh, you know, genomics on prenatal children or just at birth. It seems like there’s a, a tremendous aggregation of activities that are coming together that are almost setting up a perfect storm in not just this area, but a number of areas. I mean, I was just, I just, um, spoke to someone yesterday about fully automated whole genome analytics platform that could sort of, the information is just makes it easy to understand what’s going on. And it’s done within 24 to 48 hours soup to nuts.
David Sable: Right. We started when we started doing genetic analysis of embryos back in the mid nineties, we would take a cell stage embryo on day three, we’ve had about eight cells. We’d pluck a cell out of it, squash it down on a slide and apply a fluorescent insight to hybridization States for X, Y 13, 18 and 21. And boy, did we think we were doing hard science, like it’s, it’s so bad that I have to think down, but we discovered that we could take women that had a habitual miscarriage. They may have had five, six, seven, eight miscarriages in a row. And by choosing the genetically normal embryos, even with that incomplete asset, we could bring their miscarriage risk to answer the same as the background population. Now that was a win.
Harry Glorikian: Yeah, no, that’s that? Yeah. Yeah
David Sable: And that was late 1990s.
Harry Glorikian: It was like yesterday, relatively speaking.
David Sable: Speak. Yeah. It’s just, but yeah, you talk to the people coming out of training now, and I give talks to some of the departments, which I loved doing, and I talk about that type of technology and it’s like, yeah.
It’s like, it’s the model A.
Harry Glorikian: Yeah, yeah
David Sable: It’s yeah. It’s, it’s the Bowmore brain, you know, pocket calculator, but it’s just, it’s, it’s really, it’s, it’s fascinating to see where it’s coming, where it can go.
Harry Glorikian: Yeah. I always think of that scene in Star Trek, the original, where he says. You know, it’s like you guys are from the dark ages using leaches.
Right. I mean, it was yeah. Sort of thing. Um,
David Sable: So it’s amazing what our cultural reference points are. Yeah.
Harry Glorikian: Um, Hey, I’ve got my, I’ve got my kids watching it now with me, so I’m trying to get them. Um, w where are the biggest areas that you see right now that. Look like they’ve got the largest trajectory, ESOP, assuming, you know, things are paid for and, and, and all that from a, from a science perspective, what are the biggest areas that excite you?
David Sable: Oh, boy, I’ve got a list of 23 of them.
Harry Glorikian: Oh.
David Sable: It’s it’s really it’s the basis of my investing thesis was rather than go out and find good ideas. I wanted to define the problems first because it’s really easy to get seduced by really cool science.
Harry Glorikian: Of course. Yeah.
David Sable: So I said, no, I’ve got to be really disciplined about this and what is, what is not working.
And, you know, I came up with this list of 23 and we’re just trying to pick them off, you know, what’s the first one that, uh, was, was most timely, was frozen sample storage and tracking. Yeah, that’s the, uh, you know, we’ve been making multiple embryos each time we do IVF and for the first 15 years or so, you know, we would just put everything we had back into the uterus because so few of them turned into pregnancies and we didn’t know how to freeze them.
And then we learned how to freeze embryos. And then we learned that a freeze eggs, and we got a lot better at making embryos that could turn into pregnancy. So we got down to putting doctors one at a time. So we started accumulating tens of thousands. And now we’re into the tens of millions of specimens that are going to need to be frozen, stored, tracked, and maintained.
And it’s a problem that just kind of grew out of nowhere. Yeah. When I was doing IVF, we’d have a couple of old converted milk tanks, really cold doers, right under the, under the, under the laboratory, you know, under a bench and we’d fill it with liquid nitrogen. The straws that contained the frozen embryos had the paper labels on them sometimes, you know, handwritten, but we only had a few dozen samples.
You have a clipboard, you do inventory once every couple of weeks. And it was just, he was just kind of this sleepy little area. Fast forward to now, we’re doing embryo freezing egg, freezing specimens. You know, we’re, we’re putting back one and freezing everything else. So you’ve got rooms that have, it’s like an obstacle course of these tanks, all of which have to be inventoried.
All of which had to be maintained. The levels of liquid nitrogen. You’d have to be checked every time you need to take a specimen out, you need to navigate around the room to find it. And it’s just something, it was one of these systems that was put together with paperclip, but duct tapes, it would duct tape and paperclips.
And has we stressed it? Of course it started to break. And last year there were two very high profile lab failures where they lost numerous specimens. And some of these specimens are these aren’t for convenience. These are in some cases, people that are going to go in cancer treatment to become struggle afterwards.
And yeah. No testicular biopsies to get sperm. So you lose those that that’s, that that should be a never occurrence. So the first investment for the venture firm is to accompany that using robotics, using an RFID tagging, and, uh, you know, really brought this system into the 21st century. Interesting. It’s the true, you know, marriage of 21st century engineering, pilot, high, high level digital technology with a real need.
And you know, the, uh, the adoption of this technology is really going to be as fast as they can roll it out. Hmm.
Harry Glorikian: I was just thinking like, when you thaw you’d actually only like to thaw a certain amount of it, as opposed to all of it.
David Sable: No, it depends on what your thawing. Like if it’s sperm, if it’s embryos, if it’s eggs, you know, one of the areas that we’re trying to develop within the field are couples at high risk for serious genetic disease.
Right? Last month, uh, PBS ran the, uh, the TV version of a book. The gene-
Harry Glorkian: The gene. Yes.
David Sable: Brilliantly done. And you may remember there was an episode of this lovely family that had a child that died very early of spinal muscular atrophy or SMA, and then they would have gotten pregnant again. And, you know, it’s, it’s a, it’s a really heart-wrenching thing.
Now with IVF technology, we can, with 100% certainty, identify the embryos that are, that are safe and will not do SMA in a family like that. So what we tend to do is, you know, we recommend as an option and obviously this is correct for some couples, someone choose not to do this, but they can, uh, retrieve and, and freeze a cohort of eggs or embryos.
And that the entire family can later come from each time you want to get pregnant, you fall one, you test it. If it’s normal, you put it back. If it’s not, you don’t. Now, if you were to lose that cohort of embryos, if you’re lucky you could do it again. If you’re unlucky and the woman is no longer fertile, uh, yeah.
Then, you know, so really the technology to be able to just fall one at a time is really it’s. It’s it just preserves. The, uh, the integrity of the, all the choices that this family has to have
Harry Glorikian: Now that you’ve like jogged my memory. There’s a company, there’s a technology out of Maryland that I re I have to email you about and let you know.
But because it, it, it limits how much you thaw, um, and monitors the temperature of the sample to make sure that nothing changes, uh, specifically created for immuno-oncology. But I can see the application here.
David Sable: Sure, so it’s yeah, that’s just one example of the, you know, the 23 of the 23 actually has grown from 18.
It is from, we will be 30 by next year, all these little areas that, you know, since IVF has been such a kind of, yeah, it’s kind of cooked up in the laboratory and never standardized. There’s such a great opportunity to isolate individual interventions. And process optimize them and gradually get better and better.
But right now the best embryos created in the best laboratories have about a 65% chance of turning into a baby. Now is that 65%? Is that asymptotic because that’s where the engineering should be or is that, should it be 85? If we just find the couple of things that we don’t know that we’re doing wrong.
Right. You know, is, is, is, is a 95% embryo implantation rate. Is that like running a one-minute mile or is that just a matter of, you know, opening up a bell labs of infertility and one after another, just checking off each function within the entire IVF process and optimizing it. And that’s the fun, that’s, that’s what we’re trying to do here
Harry Glorikian: That, uh, I could almost see you as director of that Institute.
It’s not a crazy idea. I mean, it’s, it’s an area that needs to be optimized. And as you said, if you’re not looking at every single step along the way to see how to tweak it, how to improve it, if you’re expecting it to happen by itself. I mean, you’ve got to do something with purpose and drive something to change.
David Sable: Yeah. That’s, that’s what, yeah. The neat thing is a lot of people, you know, that Danielle and Helen. Two, certainly two of them are kind of attacking all these areas from different angles, but we know what we’re all kind of hamstrung with in women’s women’s health is that there’s not that many things we know how to measure, you know, what oncology, when you take pieces of the tumor and you put them into the laboratory in front of you, you can, you know, you’ve got very complex pathways that we’ve been able to define an individual enzymes and you can, you can really run very elegant, nuanced tests to see where you’re really localize, where the growth parameters breakdown, where the regulation has screwed up in, you know, the, the growth of a tumor of the growth of normal tissue. In reproductive medicine we’ve really been kind of flogging the same few hormones for 50 years. You know, there’s the hypothalamus hypothalamus, the pituitary to the ovary with a couple of detours to the adrenal. And then you see what the lighting does and what the eggs do. But the number of things we can measure is very limited. Certainly once we get into the laboratory, you’ve got the eggs and the sperm in the lab. There’s fertilization, no fertilization. There’s do you reach the cell stage? Do you reach the blastocyst stage and what are the genetic aspects of the embryo that you’ve created?
It’s a relatively limited data set. That we can draw from. So we need to come up with some really , the engineering is, is, is key. We need to kind of stretch out the science a little bit. Let’s find some new things to measure. Let’s find some pathways within the pathways that can tell us where we’re kind of driving into cul-de-sacs
Harry Glorikian: Do you think that’s because it just hasn’t been looked into, I mean, we have been digging into oncology on different levels, multiple ways. There’s, you know, I can’t, you know, you couldn’t keep up with the papers if you want it to the number of genes coming out daily is, is off the chart. Right. Um, I remember when I used to be able to at least keep them all in my head, right. That that’s, that was long gone quite some time ago.
Why do you think that we’re at this stage in reproductive health? Why aren’t we farther along?
David Sable: It’s a great question. One when the, we ponder a lot and one is, you know, kind of like studying the central nervous system, there’s only so many things you can measure safely without interfering with the process you’re trying to figure out. So you can, you know, we we’ve finally, it, it shocked us that we found that we could biopsy and embryo, uh, and figure out what the genetics are. But once that embryo goes back in, there’s almost nothing we can do to figure out what’s going on with implantation. With early development, you know, it was like, we can do ultrasounds, you know, once you hit five, you know, the five-week mark and you see the little gestational SAC and a week later, you see the heart beating with those are really just kind of, uh, benchmarks for viability.
They don’t tell you about the underlying mechanisms. Yeah, I would say, yeah, in the CNS, I want to study brain function. You know, we can do a provocative stimulus, like shine lights into the eyes or induce, you know, some type of neurologic activity. And then we do pet scans. We see which part of the brain lights up and things of that sort.
But compare that to the level of detail we get within oncology. Where we have the tissue sitting in front of us, that we can really measure specific gene expression in real time from lots of varied stimuli, under very different culture and conditions. It’s really it’s, we’re, we’re kind of hamstrung by the, these systems that nature blessed us with, with lots of protections or the CNS.
It’s not easy to do real-time study and turn inside the CNS. Right? Assuming the reproductive system holds its really protects its secrets and you know, regrets are going to chip away at it. I do think that. Doing expression studies of the embryo’s development during the in vitro phase of an IVF cycle is something that’s going to unlock a lot of secrets.
And a lot of groups are doing machine learning, applying AI. Now AI is much more a process to fighting than it is mechanistic. Yeah. It’s like the, the, you know, you and I have talked about and what Daniela went on the show, talk about Liz using machine learning for embryo assessment, using image analysis of the embryos at the blast stage, which is really brilliant, brilliant technology.
But my problem with that particular project is that it doesn’t do too much in terms of. Defining mechanism for us. And it also relies on embryos that, you know, to train the machine, to train the algorithm, you’ve got to use outcomes that are based on the old method of choosing embryos. So, uh, so like I wrote about in my Forbes paper, which most people, because I didn’t write it very clearly kind of stood huh that say, you know, we’re, we’re, we’re relying on old methods to, to generate new methods, but we, we will get there.
Harry Glorikian: No, we’re going to get blown for sure. Up I’m thinking of other, I’m already trying to think of their other methods that I’ve seen in tech where, you know, you train it, but then it starts to learn on its own of other yeah. Um, and so I think that’s going to make its way, hopefully make its way into our world.
So, so out of the other, you know, 22 that are left, which, which is the one that excites you the most?
David Sable: Well, the area clostest to my heart is using IVF to prevention, attic disease. And that’s the area with an IVF. Yeah. That’s why we started a company called Reaper genetics back in 2000. It was bought, uh, just a few years ago.
And my feeling was ultimately, this is going to be like a new area of medicine, your genetic, interventional medicine to date. We haven’t hit it. It just really hasn’t reached critical mass in one of the bottlenecks the other two, which I think is the biggest bottleneck, is that on the information area, there’s one genetic counselor for 80,000 people in the United States, which is, we just don’t have that availability to take the raw data that is, you know, you named the populations could be populations of families that have already had a tragic outcome.
They’re trying to define the risk and then define what the good options are and put that knowledge into play preventing these diseases, uh, whether it’s kind of reflexively, uh, You’re setting up a patient supply chain. A lot of these patients don’t even know this capability exists. So how do we use in almost a patient flow means taking, uh, the diagnostic data that we get from either the pregnancy or for the parents you’re testing the karyotypes.
How does that reflex into a system that has an educational loop has a referral loop. And a, uh, proliferates out into the more extended family and results in these patients showing up that we’ve been treating patients with cystic fibrosis with IVF for 20 years. Uh, very, very regularly. The only reason they show up in the clinic is that cystic fibrosis travels with male factor infertility.
And congenital absence of the vast deference is one of the hallmarks of cystic fibrosis, certain types of cystic fibrosis. So how do we do that for sickle cell anemia and spinal muscular atrophy and hemophilia, you know, all these other diseases that produce profound suffering. Get these patients into treatment.
Uh, there are other aspects that can bring that into play. It’s like one is I’d love to disassemble the IVF cycle so that we can take half of it and put it into 40,000 OB GYN offices, rather than doing it at IVF center. There’s only 1300 IVF doctors. So here we take machine learning, we feed 50,000 IVFs, stimulations, you know that the fertility drugs that we give to get multiple mature eggs at once we feed it into a. Uh, yeah, a smart computer for lack of a better term. And the computer comes up with an algorithm so that what happens with the IVF programs, either the doctor of the day, or the whole team sits around a table. And, you know, people that have been through IVF, they go in for blood tests and ultrasound almost every day.
And the results of those tests. Get analyzed each day and they come up with new orders for what, how much medication to take that night. So essentially what we’re doing is we’re doing a human version of the learning because we really make the same decisions over and over and over again. We just take a lot of time to do it, right.
Let’s build an algorithm out of the best performing clinics in the world, put it online and let the OB GYNs with the ability to access these data. The algorithm will tell them what to do for the stimulation. They can do the stimulation. The egg retrieval is a relatively simple process that any OB GYN, any OB GYN should be able to do.
And we invent a machine that does most of the embryology from retrieval the egg to through freezing it. Most of this technology exists already. Right. It a little bit of engineering work to plug that part of the lab in that way. The patient within fertility in Eastern Kansas, that doesn’t have access to a good IVF program can have that part of their procedure done with the doctor they know, and trust probably at a much lower price point done at the same level of optimization as the best clinics in the country. Then when it comes time to have the eggs thawed and fertilized and transferred, that’s when they, you know, this person can go to the IVF, you know, the IVF program,
Harry Glorikian: You know, it’s interesting that you’re saying that, and I can sort of, I’m trying to think of other areas where we’re doing something not so dissimilar, right.
That can be super imposed onto this area. If, if. If you could figure out the right business case to set up around it, to support it.
David Sable: Yeah. Well, that’s, that’s a big part of it you know, motivating us and, you know, the the, uh, the tailwinds for something like this one is that enormous population of untreated patients.
I did not make friends when I was at an industry conference in Europe a few months ago. And I was asked, he said, well, walk us through the average experience of an American. Patient with IVF. I said the average experience of an American patient with IVF is being on the outside, looking in, you’re not getting treated, right.
So let’s find ways of breaking it down to digestible parts that can be done by very highly trained people. They’re more local and it can provide it at a cheaper yet still cost-effective price, both for the supplier and for the patient. And I know that’s being done elsewhere in medicine. It’s, it’s a big challenge, but, uh, heavenly doable, you know, we’re, we’re not inventing new science, we’re just taking engineering and optimizing it.
Harry Glorikian: And I’m surprised that this isn’t more of a, you know, a drive from the. From the government itself to want to encourage this within a country. Right. It doesn’t make a whole lot of sense to me, but hey, I, you know, there are brilliant people out there.
David Sable: The government, the government does not like to get involved in IVF. It’s like a most brilliant embryologist. I know he used to say, you can get a grant. If there’s sperm in a dish, you can get a grant. If there’s an egg in the dish, if there’s a sperm in the egg and the dish together, forget it,
The NHI won’t go near it. And, uh, you know, it gets very into the politics around anything with reproduction gets extremely multi-dimensional. Right. Yeah, we really can’t. Even though there’s a lot of population reasons to want to encourage families. And certainly, you know, it’s just from a humanitarian reason, if suffering from infertility is profound suffering
Harry Glorikian: Well, and you know, again, like you said, I mean, identifying people that have the potential to have an issue in their pregnancy, a genetic issue with the child, you know, we do have ways of getting ahead of this stuff.
That can save people from all this suffering and you and I haven’t even gotten into ways to actually potentially fix some of these issues, which I think is coming. Sooner rather than later, and in a lot of different ways, David has always, it was great to talk to you. We could be talking for hours,
David Sable: –shut up about some of the stuff.
Harry Glorikian: Yeah, no, it’s it’s look, we always want to talk to people that are passionate about what they’re doing, right. That are driven by this. That’s how change happens. I, I don’t know how to do it any other way.
David Sable: I Figure I got 40 more years of work in front of me. I’m going to be probably at this for most of that time.
Harry Glorikian: Right. My wife says to me, like, when are you going to like, you know, slow down, why this is a perfect time to speed up
David Sable: Seriously.
Harry Glorikian: So, um, uh great talking to you
David Sable: I appreciate the forum. I love Moneyball medicine. Never miss it.
Harry Glorikian: Excellent. Once this pandemic is over you and I still have to go and like have a steak dinner.
David Sable: Absolutely. Absolutely.
Harry Glorikian: Okay. Looking forward to it. Take care, take care. Bye-bye
and that’s it. For this episode. If you enjoyed Moneyball medicine, please head over to iTunes, to subscribe, rate, and leave a review. It is greatly appreciated. Hope you join us next time until then farewell.